MRI in Deep Brain Stimulation for Parkinson’s Disease: Improvement of Treatment Outcomes and Precision MRI is an invaluable modality that has greatly improved treatment outcomes in patients with Parkinson’s disease. In addition, physicians are in a position to plan the placement of electrodes with greater precision, hence assuring better treatment outcomes. This sophisticated imaging technique allows more precise targeting of those regions of the brain that have been affected by the disease.
Patients with Parkinson’s disease often turn to DBS when medications no longer work well. MRI helps find the best sites in the brain to place stimulation devices so patients can receive the most benefit from treatment. Knowing the association between MRI and DBS would better inform a patient or health care provider about making appropriate choices for care.
Technology will only continue to evolve, and with it, the integration of MRI and DBS for the betterment of treatment. It brings new light to those who suffer with the debilitating concerns of Parkinson’s disease.
Key Takeaways
- MRI optimizes deep brain stimulation in patients suffering from Parkison’s.
- The effectiveness of deep brain stimulation treatment can be upgraded by accurate targeting of the brain.
- Technology advancement shaping future treatment possibilities.
Basics of MRI in Deep Brain Stimulation
While the main emphasis is placed on medical imaging, MRI has indeed become a major component in planning and monitoring DBS for Parkinson’s disease. Knowledge of how MRI works and its relations to DBS are important to optimize the treatment for the patients.
Principles of Magnetic Resonance Imaging
It produces such clear pictures of the brain by using strong magnets and radio waves. Magnetic resonance imaging depends upon the magnetic properties of hydrogen atoms found in the water and fat of the body. Hydrogen atoms in the person’s body align with the magnetic field when a person is lying inside the MRI machine.
Radio waves disturb this orientation as they pass through the body. The atoms emit signals as they return to normal. These signals are then detected and used to generate high-resolution images of structures in the brain. Abnormalities, tumors, and disorders that occur within the brain show from such images; therefore, MRI is essential to the diagnosis of ailments.
Overview of Deep Brain Stimulation
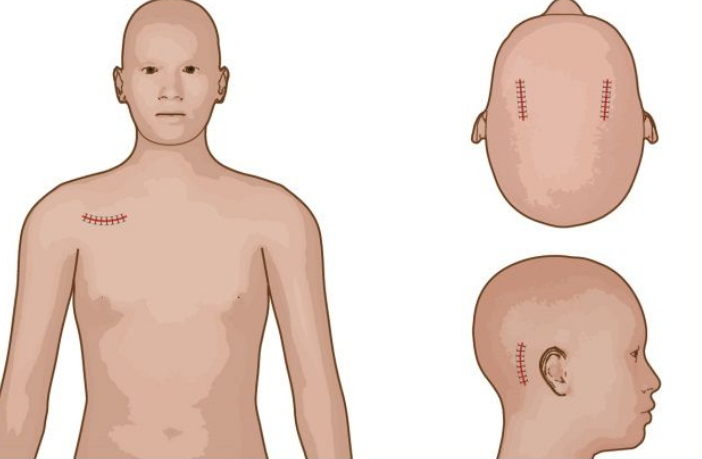
Deep Brain Stimulation: This is a surgical treatment for Parkinson’s disease. It involves implanting electrodes into specific areas of the brain. These electrodes send electrical impulses to regulate abnormal brain activity.
DBS helps reduce symptoms like tremors, stiffness, and difficulties with movement. This is especially helpful in those who do not respond well to their medications. Thus, for most, this results in a greatly enhanced quality of life.
Interaction between MRI and DBS
MRI in many ways augments the effectiveness of DBS. It helps to identify exactly in which part of the brain the stimulation should be delivered. Pre-operatively, MRI can scan a patient’s brain and identify the exact locations where electrodes need to be implanted.
Similarly, post-surgery, the position of the electrode and the response of the brain to stimulation can be followed using MRI. This ensures that treatment will be both effective and safe. It is important to understand the relationship between MRI and DBS, thereby understanding how improvement in outcomes in treatments related to Parkinson’s disease come about.
Clinical Applications and Outcomes
MRI has proved an essential component for the treatment of Parkinson’s disease using deep brain stimulation. It finds its use in planning, conducting surgery, and evaluating post-surgical outcomes. The detailed imaging with MRI contributed to every stage of the treatment.
Imaging Preoperatively for Planning of DBS
The fundamental preoperative requirement for MRI is to delineate the target areas within the brain, which usually include the subthalamic nucleus. Good images will lead to accurate planning of the placing electrode.
Key advantages:
- Anatomical Clarity: MRI provides clear images of the anatomy of the brain. It therefore enables neurosurgeons to obtain an accurate trajectory for the electrodes.
- Evaluation of Brain Anatomy: This will help the neurosurgeons assess the variational anatomy of a patient. This will allow neurosurgeons to make more precise adjustments during a procedure.
This imaging ensures effective targeting, hence providing better surgical results.
Intraoperative MRI Guidance
Intraoperative MRI can improve electrode placement accuracy at the time of surgery by enabling real-time visualization of the brain structures and thereby making adjustments in approach if necessary.
Key components include:
- Real-Time Feedback: This may enable immediate adjustments to electrode positioning, thus enhancing efficacy.
- Minimization of Complications: Precise positioning may reduce complications associated with the procedure.
- Intraoperative MRI could heighten the success rates of interventions by ensuring electrodes are optimally placed.
Postoperative Evaluation and Follow-Up
MRI after surgery helps in assessing the correct placing of electrodes and further changes in the brain over time. It is used in the follow-up of patients.
The key points to be noted are:
- Verification of Placement: MRI helps confirm electrode placement at the intended sites, a prime factor for the success of the treatment.
- Monitoring Efficacy: Brain changes due to DBS can be assessed, and therapy adjustments can be performed based on the findings.
Regular imaging helps ensure the ongoing effectiveness of the treatment and informs any further treatment plans.
Also Read :