Real-time MRI in Epilepsy Neurosurgery: The Next Step Towards Precision and Outcomes
Medical advancements continue to alter the course of treatment options available, especially in epilepsy neurosurgery. Real-time MRI technology allows surgeons to view activity of the brain and its tissues during a procedure, greatly enhancing patient outcomes. This advancement helps doctors make more precise decisions, enhancing safety and effectiveness in the surgery of epilepsy patients.
This enables surgeons to observe, in real time, changes in the brain during the procedure and hence to intervene more quickly when necessary. This is particularly important, given the complexity of brain anatomy involved in most epilepsy cases. With the integration of real-time imaging, specialists can better tailor their technique to each patient’s unique anatomy.
It means that with its development, the possibilities of neurosurgery also grow. Further research and clinical use of real-time MRI are going to be the road to new standards being set for the treatment of epilepsy and other neurological disorders.
Key Takeaways
- Real-time MRI offers a profound increase in the precision of surgery for epilepsy treatment.
- This technology immediately enables changes to be made in surgery.
- Being tailored according to the brain structure of the individual himself leads to better outcomes.
Real-Time MRI Technology Used in Epilepsy Neurosurgery
In this way, real-time MRI has become an important technology in epilepsy neurosurgery. Its contribution to improved imaging and the possibility of immediate feedback during surgery may contribute to better treatment outcomes.
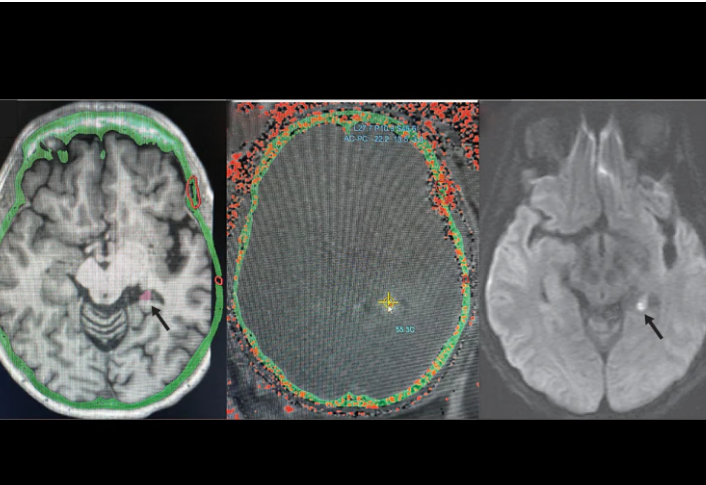
Principles of Real-Time MRI
Real-time MRI focuses on acquiring images of the brain during surgery. Advanced techniques are employed in keeping images updated, thereby continuously visualizing the motion of brain structures by the surgeon. Again, this may be quite critical in epilepsy surgery, where the issue involves precision localization of the brain tissue.
It is a technology that makes use of a rapid imaging process, hence there is a reduction of time between scans. This helps in observing the change in the activity of the brain when the patient undergoes surgery. More clear images allow making better decisions at critical junctures.
Imaging Technique Development
The resolution and speed in which real-time MRI is performed in epilepsy neurosurgery have recently undergone significant evolution. New software algorithms even further enhance image resolution and speed. These allow the imaging of even small structures with high resolution.
This modality has been further enhanced in its application by the combination of real-time MRI with other imaging techniques such as CT scans or PET scans. Such a multi-modal approach finds its application in obtaining a comprehensive view of the brain for the localization of seizure foci. Artificial intelligence is also being integrated to analyze the real-time data much more effectively.
Incorporation into Surgical Procedure
Real-time MRI incorporated into surgical settings has transformed epilepsy treatment. It allows surgeons to look at a patient’s brain in real time and improves their accuracy of removing tissue. This is particularly the case when areas of the brain involved with motor and sensory functions of the body are at stake.
This real-time imaging may instantly change the surgical strategy during an operation. The surgical team can make rapid adjustments if unexpected findings occur. Responsiveness such as this can help avoid the destruction of critical areas of the brain and enhance the safety of surgery as a whole. As this technology continues to evolve, it contributes to improved results for those undergoing epilepsy surgery.
Clinical Implications and Outcomes
Real-time MRI has important implications for epilepsy neurosurgery, ranging from an impact on patient outcomes to surgical planning and postoperative care. Advanced imaging techniques are integrated throughout the different steps of the patient’s journey to enhance precision and safety.
Patient Selection and Preoperative Planning
Patient selection is a key determinant in surgical outcomes. Real-time MRI allows for the better identification of candidates with selected forms of epilepsy, including temporal lobe epilepsy. Real-time visualization of brain structures during surgery allows surgeons to verify lesion size and location.
Besides, imaging makes it possible to forecast surgical complications that might happen. Such structural abnormalities render this technology significant since surgeons can adapt their approaches according to anatomy. Thus, seizure-free results can be highly probable.
Intraoperative Applications and Decision Making
Real-time MRI during surgery provides them with the opportunity to see the exact site right there and then. While removing the brain tissues, surgeons can view them and make appropriate on-the-spot adjustments of techniques that would cause further damage to critical areas of the brain.
For instance, when the surgeon approaches sensitive areas, real-time imaging allows for quick decisions in order to avoid debilitating crucial functions. Visualization of changes in the brain during surgery improves safety for the patient and optimizes the opportunity for complete removal of the lesion.
Postoperative Assessment and Long-Term Monitoring
Real-time MRI has also been continued into the postoperative period to assess the outcome of the surgery. It provides an immediate assessment of structures of the brain post-surgery, helping identify any complications such as hemorrhage or swelling.
Long-term monitoring is one of the features of therapy in patients with epilepsy. Repeated MRI often reveals the brain’s healing and seizure activity. This continuing assessment also supports personalized treatment plans and enables long-term outcome predictions, thus contributing to the quality of life in patients.
Also Read :