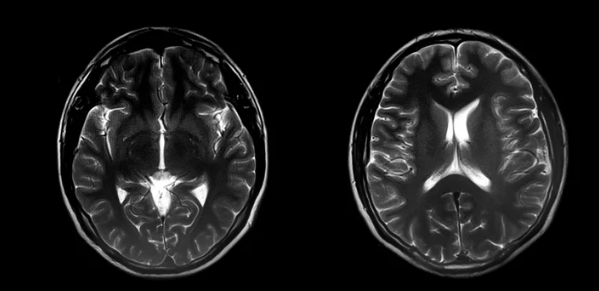
Tracking recovery after a stroke can be complicated because patients and doctors deal with a lot of detailed health data over time. MRI scans offer a clear way to see how the brain changes during recovery. Using MRI to visualize recovery gives doctors and patients direct, visual proof of progress, making the process easier to understand and manage.
MRI is a key tool in measuring damage and repair after a stroke. It helps show real changes in brain activity and structure that happen naturally or with treatment. This makes it an important part of tracking treatment success and adjusting care when needed.
Visualizing recovery with MRI can reduce confusion and motivate patients by showing their progress in a clear way. It brings complex medical information into a form that both healthcare providers and patients can easily follow every step of the way.
Key Takeways
- MRI scans provide clear images that track changes in the brain during recovery.
- Visual tools help patients and doctors understand recovery progress better.
- Monitoring recovery with MRI supports adjustments to treatment plans when needed.
Understanding MRI in Patient Recovery
MRI uses strong magnets and radio waves to create detailed images of the brain. It helps measure brain changes after injury, showing both damage and healing. MRI data guides doctors to understand recovery stages and make better treatment decisions.
Principles of Magnetic Resonance Imaging
MRI works by aligning hydrogen atoms in the body using a powerful magnetic field. When the magnetic field changes, these atoms emit radio signals. A computer collects these signals to build detailed images of brain tissues.
Different MRI techniques highlight various brain features. For example, diffusion MRI tracks water movement in white matter, revealing changes in nerve pathways critical to recovery. MRI is non-invasive and provides high-resolution images without radiation, making it ideal for repeated use in stroke patients.
Key Metrics for Assessing Recovery
MRI measures several key factors in recovery:
- Lesion size and location: Identifies damaged brain areas.
- White matter integrity: Assesses nerve fiber health through diffusion imaging.
- Axonal density and orientation: Shows nerve connections’ condition related to functional recovery.
Tracking these metrics over time helps doctors see how the brain remodels after injury. Changes in these measures can indicate progress or need for a treatment change.
Role of MRI in Treatment Planning
MRI helps design personalized treatment plans by pinpointing damaged areas and estimating recovery potential. It can assess both the core stroke site and surrounding tissues, which affect outcomes.
Using MRI scans, doctors can monitor how well treatments work and adjust rehab strategies. In some cases, changes visible on MRI inform decisions on therapies that promote brain repair or support weakened areas. This targeted approach improves patient care efficiency.
Techniques for Visualizing and Tracking Patient Progress
Patient progress is tracked using specific imaging schedules, detailed data analysis, and software tools that make results easier to understand. Combining these methods with clinical data provides a clearer picture of recovery and treatment effects.
Longitudinal Imaging Protocols
Longitudinal imaging involves taking multiple MRI scans at different times during a patient’s treatment or recovery. This approach helps monitor changes in tissues, organs, or lesions over weeks, months, or years.
Regular scan intervals are planned to capture meaningful clinical changes without unnecessary imaging. For example, scans might occur every 3 to 6 months depending on the condition. Maintaining consistent imaging settings—such as MRI sequence types and scanner parameters—is critical for accurate comparison over time.
This method allows clinicians to identify trends such as tissue healing, disease progression, or response to therapy. It also supports early detection of complications by observing subtle changes in consecutive images.
Quantitative Analysis of MRI Data
Quantitative analysis turns MRI images into measurable data. This includes calculating volumes of affected tissues, measuring signal intensities, and mapping structural changes.
Advanced software tools extract numbers from MRI scans, converting visual information into objective metrics. For example, volumetric analysis can show how much a tumor has shrunk or how much brain atrophy has occurred.
These metrics help reduce subjectivity in interpreting images and allow for statistical tracking of progress. Quantitative data can be presented as tables or graphs to compare results between sessions.
This detailed analysis offers a clearer picture of improvement or decline, supporting clinical decisions based on real data rather than just visual assessment.
Digital Tools for Progress Visualization
Digital platforms turn complex MRI data into easy-to-understand visual formats like charts, graphs, and interactive displays. These tools improve patient and provider engagement by showing clear progress indicators.
Common visualization methods include:
- Spider graphs to illustrate multiple function areas at once
- Heat maps to highlight regions of greater change
- Trend lines showing quantitative measurements over time
These visualizations help communicate recovery status quickly. They also enable better goal setting by showing where improvements are happening and where more focus is needed.
Some platforms allow patients to access their data through apps, increasing motivation by showing progress in real time.
Integrating MRI Results with Clinical Outcomes
MRI findings are most useful when combined with clinical information like symptoms, functional tests, and patient reports. This integration helps create a full picture of recovery.
Clinicians compare MRI data with patient mobility scores, pain levels, or cognitive assessments to understand how imaging results relate to actual health status. This combined approach supports personalized treatment adjustments.
For example, if MRI shows tissue repair, but symptoms remain, care plans may change. Conversely, MRI changes that match better clinical outcomes confirm treatment effectiveness.
Integrating MRI with clinical data ensures that imaging guides real-world decisions and improves patient care quality.
Also Read :