Magnetic Resonance Imaging (MRI) has become one of the most powerful diagnostic tools in oncology. Its ability to produce detailed images of soft tissues makes it invaluable for detecting tumors, staging cancer, and monitoring treatment. But while MRI provides high-quality images, the accuracy of interpretation depends heavily on best practices followed by radiologists and oncologists.
This article explores the best practices for interpreting cancer MRI scans, covering preparation, image analysis techniques, common pitfalls, and strategies for improving diagnostic accuracy.
The Importance of Accurate MRI Interpretation in Cancer Care
MRI scans are not just pictures—they are complex datasets requiring expert interpretation. Accurate analysis can:
- Improve early detection of tumors.
- Determine cancer stage, guiding treatment decisions.
- Monitor therapy effectiveness, allowing timely adjustments.
- Reduce unnecessary procedures by distinguishing between benign and malignant lesions.
Errors in interpretation, on the other hand, can lead to misdiagnosis, delayed treatment, or overtreatment.
Best Practices for Interpreting Cancer MRI Scans
1. Standardized Imaging Protocols
Interpretation begins with high-quality images. Radiologists should rely on standardized MRI protocols tailored to specific cancers (e.g., breast, prostate, brain). Consistent protocols ensure reproducibility and allow comparisons across time and institutions.
2. Comprehensive Patient History
Before reading an MRI, radiologists must review:
- Clinical symptoms.
- Previous imaging results (CT, PET, ultrasound).
- Biopsy findings.
- Family and genetic history (e.g., BRCA mutations).
This context helps differentiate between normal variations, benign lesions, and malignant tumors.
3. Use of Multi-Sequence Imaging
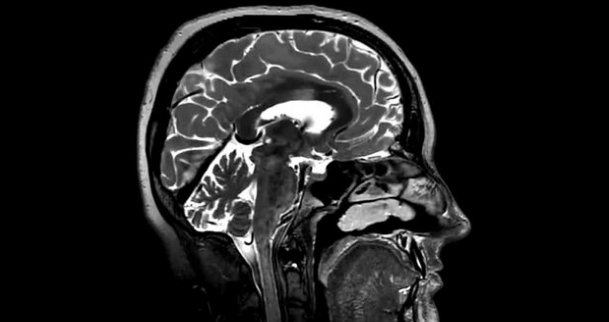
Cancer MRIs typically include multiple imaging sequences, each highlighting different tissue characteristics:
- T1-weighted images: Provide anatomical detail.
- T2-weighted images: Highlight edema and fluid.
- Diffusion-weighted imaging (DWI): Shows cellular density, useful for detecting malignancy.
- Dynamic contrast-enhanced MRI (DCE-MRI): Assesses tumor blood flow and vascularity.
Analyzing all sequences together provides a more complete picture.
4. Careful Use of Contrast Agents
Gadolinium-based contrast agents are often essential for detecting tumors and assessing their vascularity. Radiologists must evaluate enhancement patterns carefully, as these often differentiate benign from malignant tissue.
5. Side-by-Side Comparison with Previous Scans
Comparing current MRIs with prior scans helps track tumor growth, regression, or stability. This is especially important in treatment monitoring.
6. Collaboration with Multidisciplinary Teams
Interpretation should not happen in isolation. Radiologists should work closely with oncologists, surgeons, and radiation specialists to align imaging findings with treatment strategies.
7. Awareness of Normal Variants and Artifacts
Some normal tissues or benign findings can mimic cancer. Likewise, technical issues (motion artifacts, poor patient positioning) can obscure tumors. Radiologists must be vigilant to avoid false positives or negatives.
8. Structured Reporting
Using standardized reporting systems improves clarity and reduces errors. Examples include:
- PI-RADS for prostate cancer.
- BI-RADS for breast cancer.
- LI-RADS for liver cancer.
Structured reports ensure consistency and help clinicians make informed decisions.
Common Pitfalls in MRI Interpretation
Despite best efforts, errors can occur. Common pitfalls include:
- Overdiagnosis: Interpreting benign lesions as malignant, leading to unnecessary biopsies or treatment.
- Underdiagnosis: Missing small or subtle tumors, especially in early stages.
- Misinterpretation of post-treatment changes: Scar tissue or radiation effects can mimic recurrence.
- Reliance on a single sequence: Missing critical details by not reviewing all imaging data.
Improving Accuracy with Advanced Tools
Artificial Intelligence (AI) and Radiomics
AI algorithms can assist in detecting subtle lesions and quantifying tumor characteristics. Radiomics—extracting detailed features from images—provides insights beyond human visual interpretation.
Functional MRI Techniques
Advanced MRI techniques such as diffusion tensor imaging (DTI) or functional MRI (fMRI) can provide additional data for tumor mapping and surgical planning.
Continuing Education and Training
Radiologists must stay updated with the latest protocols, imaging technologies, and cancer-specific guidelines. Ongoing training reduces errors and enhances expertise.
Best Practices for Patients Undergoing Cancer MRI
While interpretation largely falls on radiologists, patients also play a role:
- Follow preparation instructions (fasting, hydration, avoiding certain medications).
- Stay still during scans to minimize artifacts.
- Provide complete medical history to help radiologists interpret findings accurately.
The Future of MRI Interpretation in Cancer
Emerging technologies will continue to improve accuracy and accessibility:
- Cloud-based imaging platforms for real-time second opinions.
- AI-assisted triage systems to flag suspicious cases.
- Global standardization of protocols to ensure quality across healthcare systems.
As these advances develop, the role of radiologists will shift from purely visual interpretation to integrating technology, patient data, and multidisciplinary collaboration.
Conclusion: Precision Through Best Practices
Interpreting cancer MRI scans is both an art and a science. By following best practices—standardized protocols, multidisciplinary collaboration, structured reporting, and the integration of advanced tools—radiologists can ensure accurate, reliable, and clinically useful results.
MRI interpretation is not just about identifying tumors; it’s about guiding treatment decisions that can save lives. As technology and expertise evolve, the future promises even greater precision and improved outcomes for cancer patients.
Also Read :