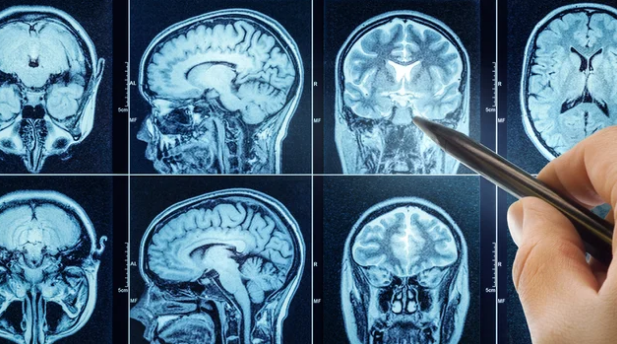
Cancer treatment has entered a new era, moving away from a one-size-fits-all approach toward personalized therapy tailored to each patient’s unique tumor characteristics. Central to this transformation is Magnetic Resonance Imaging (MRI), which provides detailed insights into tumor size, location, structure, and biology. As MRI technology advances, it is becoming a cornerstone in designing individualized treatment plans that maximize effectiveness while minimizing side effects.
This article explores the future of MRI in personalized cancer treatment, highlighting emerging technologies, applications, and the ways MRI is helping oncologists deliver more precise care.
Why Personalized Cancer Treatment Matters
Traditional cancer therapies often apply standard doses of chemotherapy, radiation, or surgery, regardless of individual tumor behavior. While effective in some cases, this approach can:
- Cause unnecessary side effects
- Fail to fully address aggressive or resistant tumors
- Delay optimal treatment adjustments
Personalized cancer treatment uses detailed information about a patient’s tumor to create targeted therapies. MRI plays a critical role by offering high-resolution imaging that guides treatment decisions and monitors responses in real time.
Current Role of MRI in Personalized Cancer Care
1. Tumor Detection and Staging
MRI provides precise imaging to determine tumor size, shape, and location. Accurate staging is essential for selecting the most appropriate therapy, whether it’s surgery, radiation, or chemotherapy.
2. Treatment Planning
Advanced MRI techniques allow oncologists to:
- Identify tumor boundaries for precise surgical removal
- Protect critical organs during radiation therapy
- Target aggressive regions within tumors for biopsies or focused therapies
3. Monitoring Treatment Response
MRI enables doctors to track how tumors respond to therapy at both structural and functional levels. Functional MRI (fMRI), diffusion-weighted imaging (DWI), and dynamic contrast-enhanced MRI (DCE-MRI) can detect changes in tumor metabolism and blood flow—often before tumor size changes are visible.
Emerging MRI Technologies Shaping Personalized Treatment
1. Multiparametric MRI (mpMRI)
Combines multiple imaging techniques into a single scan to assess tumor anatomy, function, and biology. MpMRI is widely used in:
- Prostate cancer for detecting aggressive lesions
- Brain tumors to differentiate between tumor tissue and surrounding edema
2. AI and Machine Learning
Artificial intelligence enhances MRI by:
- Automating tumor detection and segmentation
- Predicting tumor aggressiveness and likely treatment response
- Accelerating image analysis for faster decision-making
3. MRI-Guided Biopsies
MRI-guided biopsies allow doctors to target the most suspicious areas of a tumor, ensuring more accurate diagnosis and better-informed treatment planning.
4. Real-Time MRI-Guided Therapy
Some advanced systems integrate MRI directly into the treatment process, such as MRI-guided radiation therapy, enabling real-time adjustments based on tumor movement or changes in shape.
5. Functional and Molecular MRI
Functional MRI provides insights into blood flow, oxygen levels, and metabolic activity, while emerging molecular MRI techniques may identify specific tumor biomarkers non-invasively, guiding precision therapy.
Benefits of MRI in Personalized Cancer Treatment
- Higher accuracy: Improved tumor detection and targeting reduces the risk of missing cancerous tissue.
- Optimized treatment: Therapy is tailored to tumor behavior, improving effectiveness.
- Reduced side effects: Healthy tissue is spared through precise targeting.
- Early detection of recurrence: MRI can reveal tumor regrowth or metastasis earlier than other imaging methods.
- Data-driven decisions: Combining MRI with AI and other diagnostic tools provides a comprehensive understanding of tumor biology.
Challenges and Considerations
Despite its promise, several challenges exist:
- Cost and accessibility: Advanced MRI techniques and AI integration require significant investment.
- Technical expertise: Specialized training is needed to interpret complex MRI data.
- Standardization: Variations in MRI protocols across hospitals can affect accuracy and reproducibility.
- Integration with other diagnostics: Combining MRI with genetic, molecular, and biopsy data is essential for fully personalized care.
The Future Outlook
The future of MRI in personalized cancer treatment is promising:
- AI-Enhanced Precision: Machine learning algorithms will continue to refine tumor detection, predict therapy outcomes, and optimize treatment plans.
- Integration with Genomics: MRI data combined with genetic profiling could predict which therapies will work best for individual tumors.
- Minimally Invasive Treatment Planning: MRI-guided interventions may reduce the need for invasive surgeries.
- Global Accessibility: Cloud-based AI and standardized MRI protocols could make personalized cancer care more widely available.
- Adaptive Therapy: Real-time MRI monitoring may allow treatments to adapt dynamically based on tumor response, maximizing effectiveness while minimizing side effects.
Conclusion
MRI is no longer just a diagnostic tool—it is becoming a central component of personalized cancer treatment. By providing detailed anatomical, functional, and molecular insights, MRI allows oncologists to tailor therapies to the unique characteristics of each patient’s tumor.
As technology advances with AI, functional imaging, and real-time MRI-guided therapies, the future promises more accurate diagnoses, better treatment outcomes, and a higher quality of life for cancer patients. Personalized cancer care is evolving, and MRI stands at the forefront of this revolution.
Also Read :