MRI of Hydrocephalus and Neurosurgical Shunt Placement: A Comprehensive Review Hydrocephalus is a disorder of the accumulation of cerebrospinal fluid within the brain. MRI is an important modality in the diagnosis of hydrocephalus and in the selection of patients for neurosurgical shunting. This review describes the non-invasive means by which the doctor views the brain structures and provides evidence of fluid accumulation that will guide appropriate treatment.
Understanding how MRI plays an integral part in this process can help both the patient and caregiver cope with what may otherwise be a challenging surgical landscape. Learning how imaging impacts treatment options and outcomes is critical for anyone dealing with hydrocephalus. Knowing when and how shunts are placed may reduce anxiety and help communicate better with healthcare providers.
Advances in technology are in turn offering new dimensions in the use of MRI in patient care. By exploring such advancement, the reader can better appreciate how imaging techniques can eventually improve the management of hydrocephalus.
Key Takeaways
- MRI is an essential factor in the effective diagnosis of hydrocephalus.
- Accurate imaging guides neurosurgical shunt procedures.
- Understanding such processes translates into better patient outcomes.
Imaging Diagnosis of Hydrocephalus
Diagnostic imaging is, thus, quintessential in the diagnosis or management of hydrocephalus. MRI provides detailed pictures of the structure of the brain, which enables doctors to review conditions and plan treatments appropriately.
Role of MRI in Hydrocephalus Assessment
MRI is considered the gold standard for assessment in cases of hydrocephalus. It gives clear images of the ventricles in the brain where the fluid builds up, thus measuring ventricular size and structural abnormalities.
It helps differentiate types of hydrocephalus, for example, communicating and non-communicating types. Sometimes, images outline increased intracranial pressure in the effects, so they may help in the direction of treatment accordingly.
Detailed study with the help of MRI basically assesses all the surrounding structures of the brain. This comprises cerebral tissue for any damage or related condition.
Advances in MRI Techniques
Recent advances in the technology of MRI have increased the rate of diagnosis for hydrocephalus. High-resolution pictures taken from imaging studies are now clearer; thus, clinicians can better measure the size of the ventricles.
Today, functional MRI, which is done to assess activity in the brain and its blood supply, is commonly used. This may show how hydrocephalus affects brain function.
These tracts can also be visualized by DTI. So, changes in brain connectivity caused by hydrocephalus could also be estimated by using this technique. Such advanced techniques therefore not only increase the diagnostic accuracy but also bring more options for treating the disease.
Interpretation of MRI for Hydrocephalus
The interpretation for MRI studies includes certain signs in hydrocephalus. Enlarged ventricles signal an accumulation of fluid. Flattening of the cerebral cortex may be a sign of increased pressure.
This includes measurement of the ventricles by the radiologist and comparing them to normal ranges. It also includes assessment for any signs of compression of brain tissue.
If hydrocephalus is present, then treatment approach is guided by MRI findings. There will be the placement of a shunt among other interventions. For proper management of the condition, there is a need to ensure that interpretation of the images is accurate.
Neurosurgical Shunt Procedures
Neurosurgical shunting procedures are important modalities in the treatment of hydrocephalus. Procedures are used to reroute CSF to decrease intracranial pressure. The following subsections will discuss indications for shunt placement, types of shunts, surgical technique, and the approach to assessing shunt function postoperatively.
Indications for Shunt Placement
When hydrocephalus is present, the placement of a shunt is necessary due to obstructions in the flow of CSF. The most common obstructions include brain tumors, brain injuries, and congenital defects. Symptoms indicating the placement of a shunt could include headaches, nausea, changes to vision, or changes to balance.
Depending on the symptoms, a VP or VA shunt becomes indicated. The intensity of the symptoms and the imaging studies, either MRI or CT, will dictate which one is necessary. In instances where a patient has chronic symptoms, usually shunt placement is indicated for decompression to prevent future complications.
Shunt Types and Selection Criteria
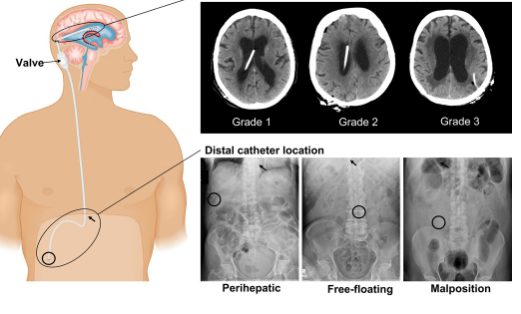
The various types of shunts used in neurosurgery include ventriculoperitoneal, ventriculoatrial, and lumboperitoneal shunts, among others. Each of these types has indications based on specific conditions.
- VP Shunt: This is the most frequently used variety. It drains the fluid from the ventricles in the brain to the peritoneal cavity in the abdomen.
- VA Shunt: It is another type of shunt that diverts CSF from the ventricles to the right atrium of the heart. This is less common and considered in diseases when abdominal drainage is not possible.
- LP Shunt: It diverts CSF from the lumbar into the abdominal region. It is more performed in patients with previous infections or after the failure of other shunts.
Type selection varies by patient health and the root cause of hydrocephalus, as well as previous treatments.
Surgical Techniques and Complications
The surgical placing of a shunt can be done through a very small usually less invasive approach. The neurologist or neurosurgeon inserts the catheter and valve system through small incisions. The length of the procedure usually ranges from about an hour to two hours; it may be performed under general anesthesia.
Even with its efficiency, complications do occur. These complications include infection, blockage of the shunt, and overdrainage. Infection may be infected in the incision or inside the shunt system. Blockage of the shunt can be treated by performing a revision to ensure functionality.
Surgeons weigh the potential risks for each patient against the benefits of surgery. Ongoing assessment of the patient’s overall condition after surgery is important since early detection of complications will make treatment easier to manage.
Postoperative Imaging and Evaluation
Imaging is important in assessing function regarding the placed shunt. MRI or ultrasound can be used to ensure that the shunt is working as it should. Follow-up will help in finding those signs of malfunction or complications regularly.
Health care providers will monitor the patient for such symptoms as headache or changes in neurological status. If new or persistent problems are identified, additional imaging or interventions may be necessary. Shunt function assessments are vital to the long-term health of the hydrocephalus patient.
Continuing communication between the patient and their respective health care team is essential for monitoring changes in symptomatology or functionality of the shunt.
Also Read :