MRI-Guided Craniotomies: A New Dimension in Neurosurgery with Ever-Increasing Accuracy The MRI-guided craniotomy is an important advance in neurosurgery. This surgical procedure allows surgeons to pinpoint and remove tumors in the brain with very minimal disturbance to healthy brain tissue. Real-time MRI imaging allows the surgeon to identify exactly how every tissue and instrument is positioned at every moment in the surgery, thus enabling precise adjustments throughout the surgical procedure.
Integrating MRI technology into surgical practice has several advantages: it enhances the identification of critical brain structures and minimizes the possibility of complications. It can be assured for the patients that this approach provides the highest level of safety and efficacy for their treatment.
Neurosurgery has been evolving over the years, and MRI-guided craniotomies are an important advancement in such evolution. Not only does the methodological approach provide an opportunity for a refined accuracy in surgery, but it also modifies the dimension of the patient’s experience. Understanding these enhancements is part and parcel of understanding neurosurgery’s future for an interested target audience.
Basic Concept of MRI-Guided Craniotomies
MRI-guided craniotomies are those brain surgeries in which the magnetic resonance imaging technique is used to increase the accuracy of such surgery. The method relies on sophisticated imaging for the location of tumors and other abnormalities within the brain with higher efficiency. The following are some of the fundamental principles and developments in this regard.
Principles of MRI Imaging in Neurosurgery
MRI relies on the use of strong magnetic fields and radio waves to produce detailed images of the brain. Unlike computed tomography, magnetic resonance imaging gives better soft tissue contrast. This is very helpful in neurosurgery, since it permits the surgeon to have a view of the structures of the brain aside from the use of destructive radiation.
There is the special type called functional MRI, which measures brain activity based of changes in the level of blood flow. It identifies those critical regions associated with speech, movement, and other functions. This way, surgeons avoid damaging such spots during surgery.
Other innovative approaches include what is called real-time MRI. Live images during surgeries have been made possible through this technology. The immediate feedback these images provide to surgeons is brilliant. They offer doctors the opportunity to change techniques right in the middle of an operation if they must, thus improving the outcomes.
Evolution of Craniotomy Techniques
Craniotomy techniques have profoundly evolved over the years. The conventional craniotomies involved greater openings in the skull, which resulted in prolonged recoveries. Newer methods use smaller incisions with advanced imaging to guide the surgeon.
Imaged-guided techniques began gaining popularity in the 1990s. These integrate pre-operative images combined with navigational systems in targeting tumors precisely while minimizing injury to healthy tissues.
These advantages mean shorter hospitalization and quicker recovery. Patients have fewer complications, hence making this option preferred when doing advanced brain surgeries.
Application in Brain Tumor Resection
The usefulness of MRI-guided craniotomy is extended in resecting brain tumors. It helps to locate tumors with precision in the brain tissue. Such accuracy enables the removal of tumors more effectively while preserving vital functions of the brain.
This technique helps both malignant and benign tumors. Malignant tumors will improve the survival by enabling the complete removal of tumors, while the benign ones relieve symptoms and improve the quality of life.
There is a possibility of real-time feedback during intraoperative MRI. This gives the surgeon an opportunity to check whether the tumor has been taken out successfully before the surgical procedure is completed. Therefore, MRI-guided craniotomies are transforming neurosurgery with better precision.
Technical considerations and workflow: MRI-guided craniotomies are a dedicated process that minimizes every type of error and makes the surgery as accurate as possible. The multi-stepped workflow takes one through various stages, from presurgical planning to real-time imaging of the procedure. Each component is integral in achieving the best possible outcome.
Preoperative Planning and Simulation
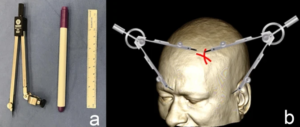
Accurate preoperative planning is carried out before the surgery of MRI-guided craniotomy. This can be achieved by surgeons through highly sophisticated imaging techniques, which deliver a very minute mapping of the brain. It highlights vital areas and structures to be avoided during surgery.
Simulation software facilitates virtual rehearsals. It allows surgeons to rehearse the procedure, making adjustments to plans based on images and foreseen challenges. Preparation this way improves coordination among team members and enhances time management in the operating room.
Salient features of this stage include:
- 3D Imaging: This provides a clear view of the anatomy of the brain.
- Risk Assessment: This involves assessing the possibility of complications given the particular anatomy of the patient.
Intraoperative MRI Integration
The integration of intraoperative MRI is the technology that allows the surgeon real-time updates on images of the brain during the course of the operation. It is an ability that is quite necessary for observing changes and shifts of the brain that may take place during the advancement of the operation.
Typically, the MRI scanner is located near the operating table. Surgeons will pause at specific, critical stages or periods for imaging. By this, they will be able to evaluate their progress and make enlightened decisions on the spot.
Key factors to note include:
- Real-time Feedback: Helps guide the surgical approach.
- Image Quality: High-resolution images are essential if proper assessments are to be done.
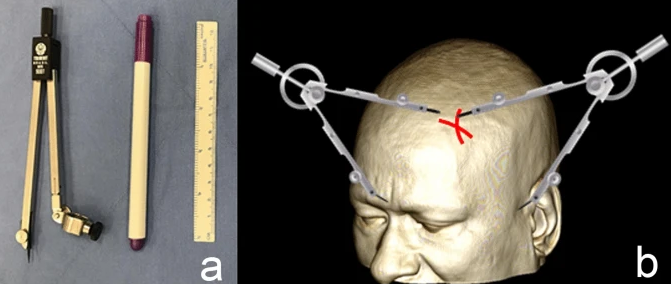
Surgical Instrumentation for Precision
Precision surgical instruments have become a necessity in MRI-guided craniotomies. Sophisticated instrumentation is currently being developed to limit further injury to surrounding brain tissue.
Instrumentation includes:
- Bipolar Forceps: These are used in coagulating and cutting tissue with minimal heat spread.
- Ultrasonic Aspirators: They help in removing tissue while preserving critical structures.
The instrumentation here mentioned works very much within the MRI environment for safety and the efficacy of the procedure. Integration of Technology and Instrumentation The integration allows for the best outcome in neurosurgical patients.
Also Read :