The Scientific Exploration of Deep Brain Stimulation in Parkinson’s Treatment Efficacy
Deep brain stimulation is a treatment that offers new hope to many people who are afflicted with Parkinson’s disease. It works by delivering electrical impulses to selected sites in the brain that assist the brain in controlling symptoms of this disorder, such as tremors and rigidity. The scientific principle behind DBS explains why the method is widely becoming an option in modern medicine.
Many patients have found relief with DBS when all other treatments have failed. This is a technique wherein a device is implanted that sends signals to targeted brain regions. For people burdened with this difficult condition, this can be very effective in improving daily functioning and quality of life.
Research continues to detail more and more about how deep brain stimulation can be individualized. The more scientists uncover the fundamentals of this technology, the better it may turn out for future patients.
Key Takeaways
- Deep brain stimulation applies electrical impulses to treat the symptoms of Parkinson’s.
- The technique has the potential to improve the quality of life in many patients.
- Ongoing research aims to enhance treatment effectiveness.
Fundamentals of Deep Brain Stimulation
Deep brain stimulation, or DBS, is among the symptomatic techniques of treatment for PD. It involves implanting electrodes in the brain to help modify symptoms. A discussion of its history, mechanisms, and neurotransmitter function in DBS is provided herein.
History of Development of DBS
Deep brain stimulation has quite interesting history. The beginnings date back to the 1950s when it was first tried as a form of stimulation of electrical impulses to the brain. Initially, DBS was used for the treatment of chronic pain.
In the 1990s, its application extended to movement disorders such as Parkinson’s disease. In 1993, the first surgery in DBS for Parkinson’s was performed. Since then, it has been widely used for those for whom medication alone is not effective. Nowadays, DBS is a well-established treatment; it improves the lives of many patients.
Mechanisms of Deep Brain Stimulation
DBS works by sending electrical impulses to certain parts of the brain. These impulses help to regularize abnormal signals responsible for movement disorders. The most common targets in Parkinson’s disease include the subthalamic nucleus and the globus pallidus.
This stimulation helps reduce the tremors, stiffness, and slowing of movements. The need for medication is also greatly reduced, with most medications causing side effects. The exact mechanisms are still being researched; however, it is known that the balance in brain activity is restored with DBS.
The Role of Neurotransmitters in DBS
Neurotransmitters are the chemicals of transmission in the brain. They play a huge role in how DBS works. In the case of Parkinson’s disease, the most significant neurotransmitter impacted is dopamine.
Dopamine itself is used in controlling movement and coordination. The loss of it in patients with Parkinson’s brings about symptoms. DBS can help because it affects other neurotransmitters like glutamate and gamma-aminobutyric acid (GABA).
It is indicated by research that these neurotransmitters interact with electrical stimulation and can further help improve motor functions. Understanding their role helps the scientists refine DBS and, by extension, treat the patients.
Clinical Applications for Parkinson’s Disease
DBS has become an important treatment modality in the management of Parkinson’s disease. It calls for appropriate patient selection, detailed surgical procedures, results evaluation, and management-all are components contributing to the successful treatment of this neurodegenerative disorder.
Patient Selection Criteria
Proper selection of patients for DBS is paramount. Typically, selected candidates have a diagnosis of moderate to advanced PD. They must have motor symptoms such as tremors, rigidity, and bradykinesia that are resistant to pharmacological interventions.
They also have to be psychiatrically and physically well enough for the surgery. They are also cognitively assessed with regard to their understanding and following of instructions after surgery. Sometimes, even younger patients with longer disease courses derive unexpected benefit from this therapy.
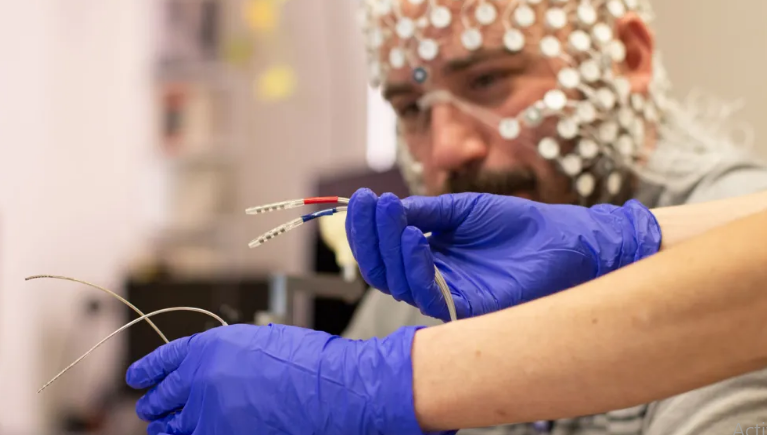
Surgical Procedure and Hardware
In DBS surgery, electrodes are implanted into the targeted region of the brain. The neurosurgeon does the surgery, usually under local anesthesia, in order for the team to monitor the patient’s response during the process.
It consists of two major parts: electrodes and a pulse generator. The electrodes are implanted deep in the brain, while the pulse generator is implanted in the chest. These can be adjusted following surgery to alter the treatment as necessary.
Monitoring the Effectiveness of Treatment
After DBS, the health professionals will reassure its efficacy regularly. Many patients considerably experience a reduction in motor symptoms. Improvement in daily activities and quality of life can be observed.
The physicians use different scales, for example, the Unified Parkinson’s Disease Rating Scale (UPDRS), to see the changes. Assessments will be carried out during the months subsequent to the procedure. Readjustment of the stimulation settings may be required to get an optimal response.
Long-term Management and Follow-up
Long-term management of DBS involves follow-ups. The patients have to attend clinics for adjustments of settings on the pulse generator. They may also require medication adjustments as symptoms continue to change with time.
Recovery and adaptation can be enhanced with support from physical therapists and occupational therapists. The patients are also encouraged to participate in support groups. It helps them in dealing with the emotional and psychological challenges of living with Parkinson’s disease.
Also Read :