MRI in Traumatic Intracranial Hemorrhage Management: Extent of Understanding Its Utilization and Effectiveness. Traumatic intracranial hemorrhage is a serious pathology that has a far-reaching complication. MRI is essential in the diagnosis and treatment of the injury; it gives clear imaging, hence allowing for better assessment of the damage to the structures. Being informed about the way MRI technology enhances hemorrhage management will support making educated decisions in critical care.
The integration of MRI has appeared to work well for medical professionals looking for effective ways to improve patient outcomes. MRI represents an imaging modality that provides detailed views of the brain and thus assists in intervention planning in a very fast way. The versatile applications of MRI have been continuously developing and shaping the world of emergency medicine.
The necessary insights into the potential benefits that MRI offers to trauma patients and their families can help them so much. It can make all the difference in the recovery process if they can be informed about how this precious modality can lead to timely interventions.
Key Takeaways
- MRI enhances diagnosis related to traumatic intracranial hemorrhage.
- It aids in planning appropriate treatment options.
- Understanding the role of MRI results in better patient care and outcomes.
Role of MRI in the Diagnosis of Intracranial Hemorrhage
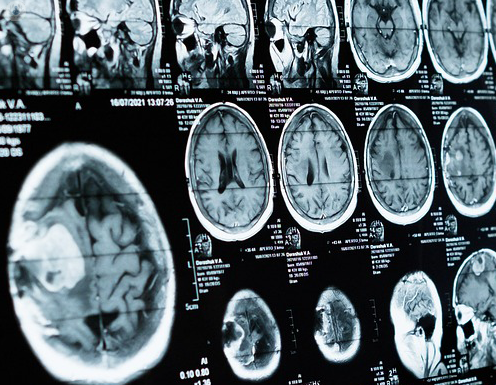
MRI serves a critical diagnostic role in intracranial hemorrhage. MRI provides detailed images of the structure of the brain that aid in diagnosis through the detection of bleeding and the extent of the bleeding. This section covers the basics of MRI imaging, advantages over CT scans, and MRI techniques innovations.
Basic Principles of MRI Imaging
MRI applies powerful magnets and radio waves to generate images of the brain. It is specially helpful in the detection of hemorrhages: subdural, epidural, and intraparenchymal bleeding.
MRI does not use radiation; hence, it is also safer for the patients than X-ray computed tomography. The method produces high-resolution images, reflects the changes in brain tissues, and blood flow. It will outline abnormalities that may well not be visible on other imaging techniques; thus, diagnosis will be correct.
MRI vs. CT: Advantages in the Detection of Hemorrhage
Although most common in emergency situations is the use of CT scans, there are certain advantages to MRI. MRI is more sensitive for certain types of hemorrhages and the ability to capture images in multiple planes. This outlines small bleeds that may have been missed on a CT.
MRI is also more sensitive in defining blood product type: it can differentiate between fresh blood, older clotted blood, and other fluid collections. This may be crucial in determining optimal treatment for the patient.
Recent Advances in MRI Techniques for the Evaluation of Hemorrhage
Recent advancements in MRI techniques have further strengthened the assessment of hemorrhage. With a variety of techniques, such as DWI and SWI, subtle hemorrhages are now detected more appropriately.
DWI is very good at the diagnosis of acute strokes, while SWI is sensitive to microbleeds. These enable the physician to diagnose earlier and more accurately. They support the physician in making informed decisions regarding treatment and the management of the patient for improved outcomes.
Incorporating MRI into the Management of Hemorrhage Protocols
The application of MRI in traumatic intracranial hemorrhage provides a wealth of information useful to guiding treatment options. Improved patient outcome depends on the use of advanced imaging better in protocols.
Case Studies: MRI-Guided Treatment Decisions Various case studies in clinical practice demonstrate the way MRI helps in making treatment decisions for trauma cases. One such case study is that of a patient who had a subdural hematoma. MRI delivered information on the size of the hematoma as well as the implication of its size on the brain tissue surrounding. This information helped the medical team to make a decision as to whether the case needed surgical intervention.
In another case, MRI explained a patient’s condition with an epidural hematoma. The imaging revealed possible complications that could not be visualized using a CT scan. This allowed surgical management in good time and greatly improved the prognosis of the patient.
These cases show how MRI is important in clinical decision-making because it aids in the determination of specific treatment modalities for effective management of patients.
MRI after Treatment: Follow-up and Prognosis
It would be necessary to follow up the case of traumatic intracranial hemorrhage with an MRI after treatment. The MRI provides detailed images that enable residual hemorrhage or new complications to be assessed visually. It helps in assessing the efficiency of the initial treatment plan given to the patient.
For example, if the MRI scan of a patient post-treatment still reveals bleeding, then the treatment strategies can immediately be changed by the medical teams. MRI also aids in long-term outcome prediction. Various studies have identified that some MRI findings are associated with the possibility of recovery and complication rates.
The application of MRI in this regard helps in proactive management of the patients and provides every opportunity for good recovery.
Also Read :