MRI-Based Radiomics in Neurosurgical Outcome Prediction: Advancing Precision Medicine The approach of MRI-based radiomics is becoming a game-changer in the ability of neurosurgeons to predict the outcome for patients. This innovative strategy underlies the analysis of MRI scans to identify certain patterns that may help in estimating recovery and potential complications. Such imaging data, with the use of sophisticated algorithms, is turned into precious knowledge that helps in surgical decision-making.
Acquiring such patterns signifies much in improving patient care. In that respect, MRI-based radiomics will investigate the characteristics of tumors and brain structures in detail for personalized predictions of patients. This will further help neurosurgeons with more effective treatment plans and improve prognosis accordingly.
With its continuous evolution, this technology plays an even more vital role in neurosurgery. Today, professionals seek to introduce such tools into everyday practice in order to achieve better results and an individualized attitude toward patients.
Key Takeaways
- MRI-based Radiomics: It provides a prediction of neurosurgical outcome influenced by the findings.
- The study of imaging patterns leads to better decisions regarding treatment planning.
- This technology, while developing, has an increasingly important place in modern neurosurgery.
Principles of MRI-Based Radiomics
MRI-Based Radiomics: It involves the extraction of more detailed information from MRI scans to help predict surgical outcomes in neurosurgery. The basic components involve principles of MRI technology, workflow for analyzing radiomic features, and the process of data acquisition and standardization.
Principles of MRI Technology
MRI relies on a strong magnetic field and radio waves to yield well-detailed images of the body. Essentially, it depends on the principles of nuclear magnetic resonance, an approach that detects signals from hydrogen atoms in water molecules.
Typically, the MRI machine generates images in sagittal and axial planes. The whole process is rather rewarding in determining structural defects in the brain. Magnetic resonance imaging applies several types of sequences such as T1-weighted and T2-weighted images, which provide different contrasts of outlining various tissues.
These images form the basis for radiomics, where the focus of analytical efforts has now moved toward features quantification that might predict patient outcome after neurosurgery.
Radiomics Workflow and Features
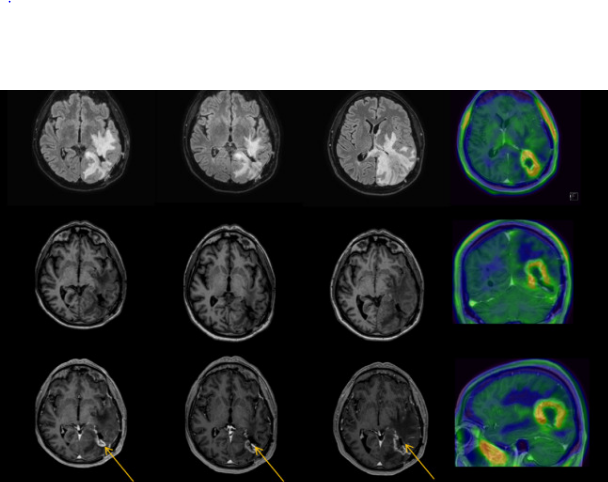
The general steps of most radiomics workflows include image acquisition, feature extraction, and analysis. Subsequent to MRI scan acquisition, several software applications identify salient features in these images, including those that define shape, texture, and intensity.
Feature extraction hence yields a very large data set from which patterns may emerge that could hardly be detected with the naked eye. First-order statistics, describing the distribution of intensity values of the pixels of an image, as well as higher-order features characterizing spatial relationships between pixels, are some of the most salient features.
Statistical and machine learning analysis of these extracted features allows one to predict treatment responses and outcomes, which is important for personalization of care for individual patients.
Data Acquisition and Standardization
Data acquisition is a very critical aspect for any kind of successful radiomics analysis. Standardization of MRI scanning protocols provides consistency in the images taken at different times and varied centers. The type of scanner, field strength, and sequences applied should be standard.
Standardization of image data also entails steps involving image preprocessing. These may include normalization of images, resizing, or removal of noise. Appropriately standardized data enhances the reliability of the features extracted.
This will be further facilitated through collaboration between the clinical teams and imaging specialists to establish best practices. Such a process leads to increased quality of the data, thus enabling the better prediction of neuro-surgical outcomes.
Application in Neurosurgery
The important role of MRI-based radiomics is that it finds its application in neurosurgery. Imaging data analysis helps in the understanding of brain tumors, guiding surgical decisions, and predicting outcomes.
Preoperative Analysis
MRI-based radiomics in preoperative analysis enables detailed imaging features of brain tumors, hence characterizing tumor type, grade, and infiltration level.
Subtle differences may be picked out by radiomic features like measurements of texture, shape, and intensity. Such information helps neurosurgeons to decide on the best surgical strategy. Such data can result in more precise targeting of tumor regions and the avoidance of critical structures.
Moreover, radiomics can be combined with clinical data to further refine diagnosis. It enhances the classification of tumors, which could affect treatment decisions.
Surgical Decision
Radiomics based on MRI during surgical decision-making supports surgical risk assessment. It aids neurosurgeons in the decision regarding the extent of resection by predicting tumor behavior.
For instance, if the radiomic features point to a high risk of recurrence, then the surgeon can be more aggressive. More realistic predictions ensure patient safety and further guarantee better surgical outcomes.
Radiomic information can heighten collated discussions among the surgical team. Representations of complex imaging data assist in deliberating the different benefits as well as risks associated with a given case.
Prognostic Estimation and Risk Assessment
MRI-based radiomics significantly improves prognosis and risk estimation. Radiomics signatures provide insights into the likelihood of patient recovery or complications.
Radiomic features postsurgery will assist health teams in identifying complications much earlier, thus enabling appropriate follow-up care and monitoring.
Radiomics could also give better estimates of survival rates and recurrence risks. That kind of knowledge will help the patients and clinicians set realistic expectations and prepare for future treatments.
Also Read :